
For providers with the strongest histories of evidence-based practice, the program will eliminate clinical review requirements for the duration of the pilot. Under the program, providers with a history of excellence in adhering to evidence-based clinical pathways will be able to submit their advanced imaging requests via a streamlined process that substantially reduces their administrative burden. The Provider Passport Program was developed from valuable feedback from the provider community regarding the prior approval (PA) process. The program sets to simplify the process for participating providers to order MRIs, CAT scans, and other forms of radiology for patients, which should also speed up access to care for patients. The Provider Passport Program for Advanced Imaging is part of our ongoing commitment to improving quality of care for our members while reducing administrative burden for our network providers. To look up out-of-area member's prior approval/pre-notification/pre-certification/pre-service requirements, please use the Medical Policy Router on the Provider Polices page. Inpatient Rehabilitation Continuation Worksheet.Initial Inpatient Rehabilitation Worksheet.Census Reporting Requirements and Process.If calling, have the member name and certificate number ready, as well as the clinical details. Call us directly for a pre-notification request.
AIM SPECIALTY HEALTH PRIOR AUTHORIZATION FAX NUMBER DOWNLOAD
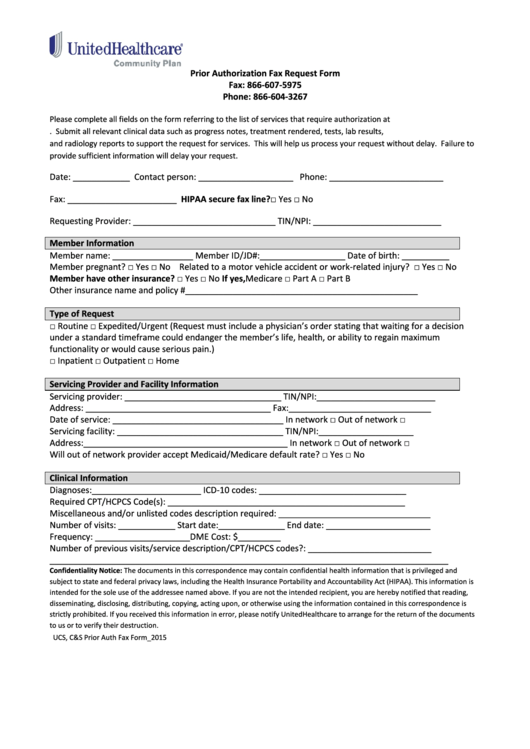
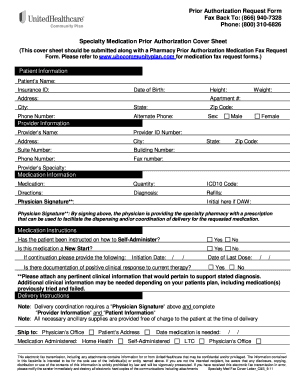
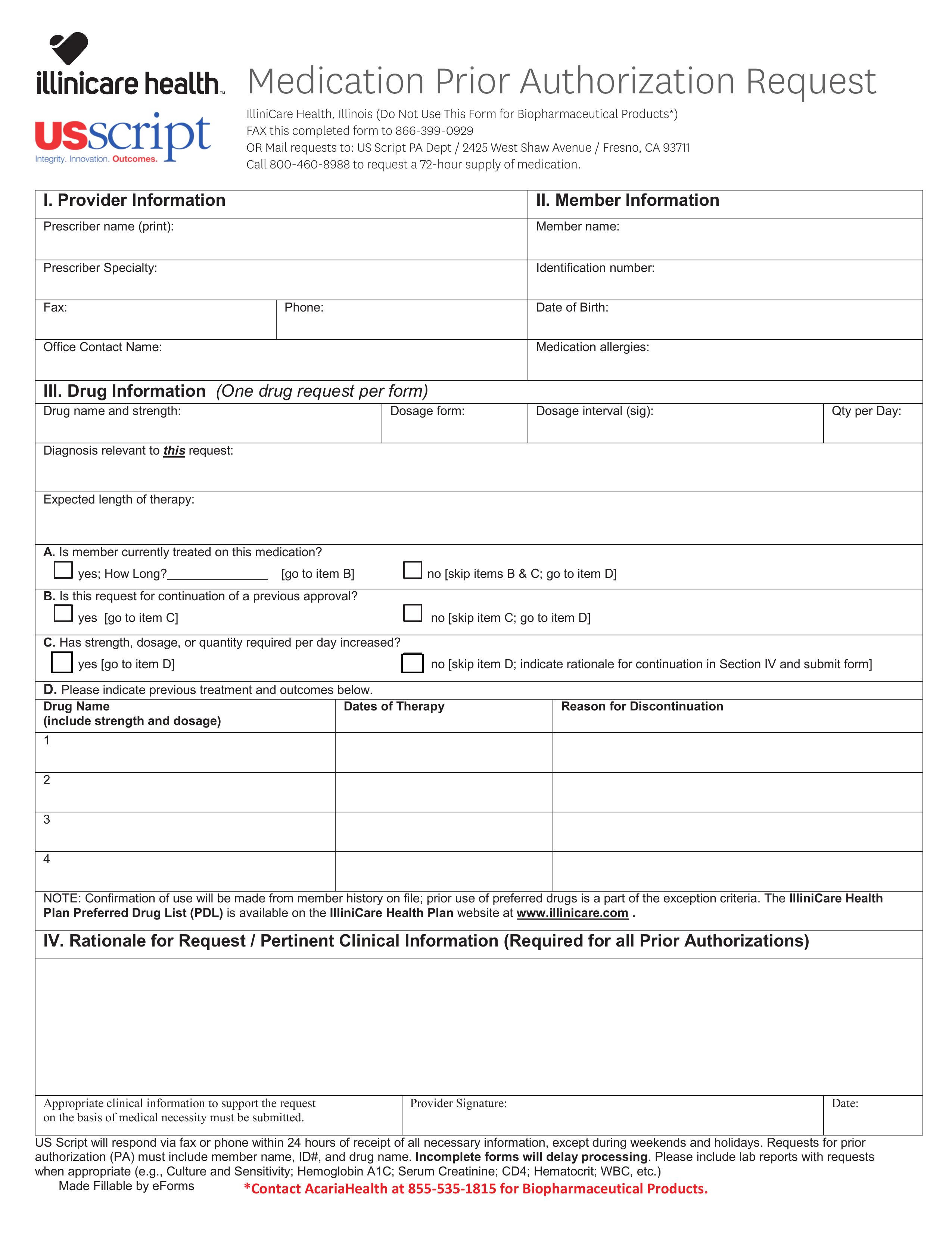
Download the prior approval form fax the completed prior approval form(s) to (866) 387-7914.Submit pre-notification requests electronically via Acuity Connect by logging in to the Provider Resource Center.You can complete pre-notification in one of three ways: Providers are verbally notified of the determination of pre-notified services within three business days after obtaining all necessary information. The information is reviewed in conjunction with nationally recognized health care guidelines. We collect clinical information pertinent to the admission request. Pre-notification is a review conducted by Blue Cross and Blue Shield of Vermont before a member's admission to a facility for inpatient care, to confirm the appropriateness of the requested level of care and to assist with discharge planning and coordination of care for services not requiring prior approval. To look up out-of-area member's prior approval/pre-notification/pre-certification/pre-service requirements, please use the Medical Policy Router located on the Provider Policies page. Quick Tips Sheet for using the searchable prior approval database.2023 Federal Employee Program List of Prior Approval Requirements for FEP Blue Focus.2023 Federal Employee Program List of Prior Approval Requirements for Standard and Basic Options.2022 Federal Employee Program List of Prior Approval Requirements for FEP Blue Focus.2022 Federal Employee Program List of Prior Approval Requirements for Standard and Basic Options.Drugs Requiring Prior Authorization in the Medical Benefit.Services, Equipment & Supplies Requiring Prior Approval.Facts and Tips on the State of Vermont Uniform Medical Prior Authorization Form.Use CoverMyMeds (Member ID should include the last letter (usually V) followed by twelve numbers and the two-digit member number).


 0 kommentar(er)
0 kommentar(er)
